Have you been diagnosed with keratoconus? It’s estimated that approximately 1 in 400 people have this condition.
Keratoconus affects the shape of your cornea and your ability to see. Most treatment options aim to restore your vision for today but may not prevent the progression of keratoconus in the future.
One treatment has the power to impede the development of this disease and decrease the chances of further vision changes. Keep reading to learn more about keratoconus and how corneal cross-linking can treat this eye condition!
What Is Keratoconus?
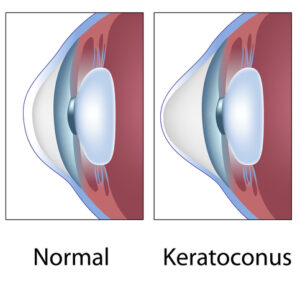
Keratoconus refers to a thinning of the cornea, which then bulges outward. The cornea is found at the front of the eye and is responsible for focusing light so you can see clearly.
A healthy cornea should be clear and dome-shaped. When keratoconus occurs, your eye cannot focus properly, causing blurry and distorted vision.
In most cases, this condition begins to develop when an individual is in their teens or early 20s. It is common to be asymptomatic in the early stages.
Keratoconus typically takes years to progress. Patients may begin to notice symptoms including:
- Distorted vision
- Light sensitivity
- Halos
- Eyestrain
- Redness
- Poor night vision
- Nearsightedness or astigmatism
- Excessive eye rubbing
- Finding it more challenging to wear contact lenses as the condition progresses
The exact cause of this condition is unknown. It may have a genetic component, meaning it’s often passed down through families.
Certain disorders may increase your likelihood of developing keratoconus. These include allergies, Marfan syndrome, and Down syndrome. Your chances of developing keratoconus may increase if you excessively rub your eyes.
Collagen in the eye allows it to hold its spherical shape. These protein fibers can weaken and affect how the eye keeps its shape. If the eye’s shape becomes affected, this results in a corneal bulge.
Your eye doctor can detect keratoconus by conducting an eye exam with diagnostic imaging designed to map out the contours of the front of your eye. This diagnostic imaging is referred to as corneal topography. Your doctor will monitor your corneal topography on a regular basis to determine if there are any signs of progression.
How Has Keratoconus Traditionally Been Treated?
The goal of treatment for keratoconus has been to restore clear vision. How your eye doctor chooses to treat keratoconus depends on your symptoms.
These indicate the severity of the condition and the speed of its progression. Many eye doctors begin treating keratoconus after an initial diagnosis using prescription glasses or contact lenses.
In most cases, this is effective when the condition is in its early stages, and symptoms are mild. Prescription changes may be needed as the condition continues to progress.
Hard contact lenses, or rigid gas permeable contact lenses, are commonly prescribed. They assist in reshaping the cornea while preserving the flow of oxygen into the eye.
The downside of this type of lens is that some patients find them uncomfortable. If rigid gas permeable contact lenses are too uncomfortable, scleral lenses are one option that may be more comfortable than other kinds of lenses.
By providing a liquid layer between the lens and the surface of the eye, they can minimize distortions to your vision. They may not be as bothersome to wear as they rest on a less sensitive part of your eye than other lenses.
When other treatments are not enough, corneal transplants may be recommended in severe cases. This procedure involves surgery that replaces the cornea with a healthy one from a donor.
What Is Corneal Cross-Linking?

Traditionally, patients had no choice but to wear hard lenses or undergo surgery to treat their keratoconus. Now, a revolutionary treatment is changing patients’ lives and saving their vision.
Corneal cross-linking is the only treatment that can slow down the progression of keratoconus. While it can’t reverse any changes that have already occurred, its goal is to prevent further changes to your cornea and the worsening of your vision.
Dr. Dell was the first surgeon in Austin to offer cross-linking as a treatment option for keratoconus. He also served as the chairman of the first national meeting on corneal cross-linking in the country.
Dell Laser Consultants has treated more patients in Central Texas using corneal cross-linking than any other clinic, thanks to our FDA clinical trials, which allowed us to offer this technology before it was FDA approved.
How Does Corneal Cross-Linking Work?
During corneal cross-linking, your eye doctor instills eye drops containing vitamin B2 (or riboflavin). This solution is sensitive to ultraviolet rays.
Then, they expose your cornea to UVA light for 30 minutes or less. The UV light activates the riboflavin.
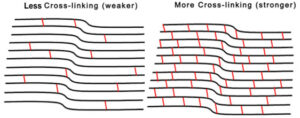
The riboflavin creates bonds (known as cross-links) between the weakened collagen fibers in the eye. Cross-linking the collagen fibers strengthens them and halts further thinning, so they can hold the shape of the eye again.
The procedure is pain-free and takes only 60 to 90 minutes. Your eye doctor places a contact lens that acts as a bandage over the eye. You’ll be able to return home the same day.
For many patients with keratoconus, having a procedure like corneal cross-linking means they don’t have to undergo a corneal transplant in the future.
Results of the procedure have demonstrated they are long-lasting. Studies have shown that in 95% of patients, the progression of keratoconus stopped. Between 60-70% of patients have also reported improvements to their vision after having corneal cross-linking.
Are you looking to stop the progression of your keratoconus? A keratoconus diagnosis doesn’t have to mean continued worsening vision.
Find out if you’re a good candidate for corneal cross-linking by scheduling your appointment at Dell Laser Consultants in Austin, TX, today!