What you need to know about Dry Eye
- It is estimated that as many as 50 million Americans suffer from dry eye syndrome.
- Dry eye syndrome is a chronic disease that impacts the quality of life of affected individuals.
- Although you can get dry eye at any age, there is an increased risk with age.
- Wearing contact lenses increases the risk of dry eye syndrome.
Dry eye syndrome is the most common pathology that affects the eyes. It can be difficult to diagnose because it can present in dramatically different ways. Signs and symptoms associated with dry eye include burning, grittiness, stinging, red eyes, light sensitivity, decreased night vision, and even an overall decrease in vision. Many dry eye patients experience some degree of decreased vision—like driving around with a dirty windshield.
Healthy Eye

Dry Eye

Some of the less obvious signs of dry eye include itchy eyelids, fluctuating vision, decreased contact lens wear time, and even tearing of the eyes. Dry eye tends to get worse with age and can lead to sight-threatening complications. Most patients are subtly bothered by dry eye, but if left untreated, it will likely get worse over time.
Treatment of dry eye is much more complex than using artificial tears and can be as invasive or as surgical reconstruction of the eyelids. Dry eye must be addressed and treated prior to keratorefractive surgery, such as Austin LASIK Surgery and cataract surgery. Treatment of dry eye is usually simple and well tolerated but can make a world of difference in one’s everyday life.
The Dell Eye Institute for Dry Eye Research at Dell Laser Consultants is proud to be the only comprehensive dry eye clinic in Central Texas and a national leader in the field.
The Dell Eye Institute For Dry Eye Research

Want to Learn More About Dry Eye?
Interested in learning more about Dry Eye? Please click the button below to contact us!
Contact UsThe Complexity of Dry Eye Syndrome
Dry Eye sounds like a simple term, but it is a complex and sometimes poorly understood disease. Even amongst eye care specialists, there is significant confusion because what a patient feels often does not always correlate with what the doctor sees upon examining the patient.
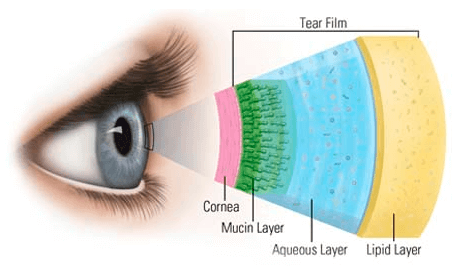
The tear film is a remarkably complex structure that combines essential fatty oils, water, proteins, electrolytes, and vitamins. Tear film cleans the eye, provides infection control, hydrates tissues, nourishes the cornea, lubricates against blink friction, and even serves as one of the most important optical surfaces for vision. The human cornea has one of the highest metabolic rates in the human body, but it has no blood supply; it relies on obtaining all of its nutrients from the tear film.
The tear film consists of three unique interactive layers:
- The lipid (oil) layer is produced by approximately 45 glands, which line the edge of each of your eyelids. This layer of the tear film is responsible for preventing dehydration and evaporation of the tears, increasing the quality of vision, and allowing the tear film to vertically cover the eye despite gravitational forces. Dry eye secondary to a deficient lipid layer is the most common form of dry eye and may represent as much as 85% of all dry eye patients. This type of dry eye may also be accompanied by red and swollen eyelid margins, eventually leading to the loss of eyelashes. Conditions closely associated with lipid deficiency include poor diet, contact lens wear, fair skin, and age. Treatments can range from oil-containing eye drops to nutritional therapies such as omega-3 fatty acids to heated automated expression of the eyelid glands. Currently, the most advanced procedures involve thermal expression of the eyelid glands or the use of intense light pulse therapy (IPL) to increase gland expression.
- The aqueous (water) layer is primarily produced by the lacrimal gland, which is located on the outside corner of the upper eyelid. Dry eye secondary to a deficient aqueous layer is closely linked to hormonal variation, oral medications, increased age, female gender, and poor diet. This type of dry eye can be treated with medicated eye drops and plugging of the tear ducts.
- The mucin layer is produced by conjunctival cells on the white part of your eyes and provides the base for the rest of the tear film to adhere to. Mucin deficiency can lead to a complex form of dry eye for which medicated eye drops as well as oral therapies may be needed.
How is dry eye diagnosed?
The historical problem with dry eye is that what a patient feels rarely matches what the doctor sees upon examining the patient. This has lead to much confusion in the past and the missed diagnosis of dry eye syndrome. Like many other chronic diseases, the disease state can often be present for years before a patient starts to suffer significant effects. Furthermore, many patients suffer from dry eye syndrome in conjunction with other diseases, such as blepharitis, contact lens intolerance, ocular rosacea, seasonal and environmental allergies, and various systemic conditions. By utilizing the most advanced technology, our physicians are able to identify underlying causes or other disease factors that may be contributing to dry eye symptoms.
Testing at the Institute for Dry Eye Research at Dell Laser Consultants includes:
- Infrared gland imaging
- SPEED™ dry eye questionnaire
- Tear film osmolarity testing
- Sodium fluorescein corneal staining
- Lissamine green conjunctival staining
- Tear meniscus evaluation
- High contrast digital corneal lipid layer analysis (LipiView®)
- Digital blink analysis (LipiView®)
- InflammaDry® ocular biomarker testing
- Corneal topography mapping
- Ocular allergy testing (customized for Central Texas allergens)
- Lactoferrin protein tear testing
- IgE immunoglobulin tear testing
- Sjö™ Sjogrens syndrome testing
- Schirmer tear production testing
- Tear break up
- Corneal epithelial cell OCT mapping
No single test alone is adequate for establishing the diagnosis of dry eye. Results from multiple tests will add to our experienced physicians’ understanding of an individual’s specific condition in order to customize a treatment plan.
The Dell Eye Institute for Dry Eye Research at Dell Laser Consultants philosophy for treating dry eye
All patients with dry eye syndrome receive personalized treatment plans tailored to their needs. In general, the earlier dry eye syndrome is diagnosed, the more responsive it is to treatment. All dry eye results in ocular inflammation and our priority is to first include the inflammation and secondarily reduce the burden of this disease on your life.
The Dell Eye Institute for Dry Eye Research at Dell Laser Consultants can provide patients with all of the advanced dry eye therapies available in the United States. Our research and dry eye experts also have access to many products and therapies that are not yet commercially available in the United States through our participation in FDA-sponsored clinical trials. We make all of these resources available to our patients to ensure world-class medical care.
Available Dry Eye Therapies Include:
Artificial tears, gels, and ointments

Tear supplementation is a mainstay of the traditional management of dry eye. Current research suggests that
artificial tears do little more than provide momentary relief from symptoms. Unfortunately, artificial tears do not
address the root cause of any dry eye issue and are therefore not considered a conventional treatment of dry eye but rather just a momentary relief mechanism. Artificial tears, gels, and ointments temporarily improve the optical quality of the tear film, alleviate symptoms, facilitate adequate spreading of oil gland secretions, and increase the lubrication between the eyelid wiper and the ocular surface. The goal with all dry eye treatments is to get the body to produce more of its own nutrient-rich tears rather than just coat the eye with non-specific saline for minutes. Our physicians will provide specific recommendations based on the patient’s needs.
Intense pulsed light (IPL) therapy
This is arguably the most popular dry eye treatment available worldwide now. The use of IPL for dry eye was pioneered in the US by both Dr. Dell and Dr. Cunningham in 2015. Before 2015, IPL was primarily used as a cosmetic therapy. The FDA trial and current national treatment protocols were developed right here at DLC. These protocols are now followed worldwide from academic institutions to the leading treatment centers. At DLC our physicians have access to multiple IPL technologies and devices that can both optimize dry eye therapy and cosmetic outcomes.
Intense Pulse Light (IPL) creates photothermolysis (heat generated from light to destroy cells) by emitting short wavelength polychromatic light in millisecond pulse duration using wavelengths of 500-1200nm to treat facial skin damage, including wrinkles, coarseness, laxity, dyspigmentation. For dry eye, the objective is to deliver selective energy targeting dermal vascular and pigmented lesions to improve tissue surrounding the lids and meibomian glands to minimize vascular leakage of inflammatory mediators and ablate abnormal vessels.
Typical treatment courses involve 4 treatments separated by 2-4 weeks and may be more beneficial if the entire face is treated rather than just the upper cheek area.
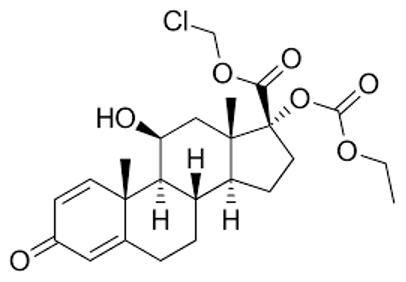
Steroid Eye Drops
Steroid eye drops are often used to both initiate dry eye treatment and manage subsequent flares. At DLC we use special steroid eye drops that have much less chance of causing any ocular side effects than traditional steroids. These steroid eye drops also have no systemic absorption and can safely be used with other medications.

Xiidra, Cequa, and RESTASIS® prescription eye drops
These are immunomodulatory eye drops that reduce inflammation and increase the eyes’ natural ability to produce tears. They are very safe for long-term use and have no known systemic drug interactions. They are long-term therapies and may take months to become effective.
Punctal Plugs (Eyelid Drainage Plugs)
These minimally invasive plugs can be thought of as a drain stopper that goes in a sink. They recirculate and maintain more of your body’s nutrient-rich tears in the eyes, often decreasing or eliminating the need for artificial teardrops. They are painless and take less than one minute to place (usually in the drainage canal that is located in the lower eyelid by the nose). Both temporary and permanent plugs are available. Temporary plugs will dissolve like a sugar cube while permanent plugs are long lasting and made of plastic. Both types of plugs are so small that they are not visible to the naked eye.
TearCare®
TearCare® is the latest device developed to evacuate stagnant, clogged meibomian glands. It is an in-office treatment that takes only 15 minutes and is minimally invasive.
A study published in 2022 in the journal Clinical Ophthalmology showed TearCare® to be superior to Lipiflow in the treatment of dry eye.
In 2023 Sahara study showed TearCare® to be superior to Restasis in the treatment of dry eye.
LipiFlow® Treatment

This computer-automated 12-minute treatment heats up and massages the eyelid glands in order to express their contents and reduce retained inflammatory factors. This treatment is unique, as the heat is applied to the inner lid surface directly over the oil-producing gland. In affected patients, this treatment has been shown to reduce ocular dryness symptoms for up to 18 months. Many patients receiving this treatment are able to eliminate prescription medications for dry eye such as RESTASIS®.
BlephEx™ Eyelid Treatment
This treatment removes debris and blockage from the eyelid gland openings on the margin of the eyelids. It leaves eyelids and lashes looking much more natural and healthy. It has been shown to relieve dry eye symptoms in affected patients for up to six months and can often extend the symptomatic relief of TearCare®, IPL, or LipiFlow® eyelid treatments. In the same way a dental hygienist can clean your teeth much more effectively than you can ever brush them at home, our lid hygienists can use this technology to remove debris, oily secretions, and bacteria from the eyelid margin. This treatment can also be used prior to cataract surgery in order to decrease the risk of infection and/or inflammation.
Consistent heat therapy eye masks
The application of heat to the eyelids is implemented by using warm compresses, a facemask, goggles, or similar device. It was thought that elevating the temperature of the eyelids can unclog oil-producing glands at the base of the eyelids in order to release necessary oils into the tear film. Recent studies have shown that heat masks are likely not effective at heating meibum and the applied heat increases dry eye-related inflammation. Heat masks are a therapy that may help a small segment of dry eye patients but in general, are now avoided in dry eye therapies due to heat’s negative effects on inflammation.
Eyelid hygiene wipes
These wipes help clear debris from the base of the eyelashes and help to open up the oil-producing glands at the base of the eyelashes.

Nutritional therapies
Several foods and nutritional supplements have been shown to help dry eye and re-establish a healthy ocular surface. We will detail what commonly available supplements will help to alleviate a patient’s dry eye symptoms.
Lifestyle alterations
Daily activities can affect one’s ocular comfort. Everything from medication usage to workplace ergonomics can have a significant effect on eyes. We will guide patients through simple changes in their day-to-day activities that will help alleviate dry eye symptoms.

Hypochlorous Acid Spray
This is a safe and effective spay that is both antimicrobial and anti-inflammatory when used on the eye lid and eye lashes.

MIEBO™
MIEBO™ is a preservative fee, drug free, synthetic oil prescription eye drop that has been shown to be effective in treating dry eye. The proposed mechanism involves reducing desiccation stress on the cornea.

Tyrvaya
This is a neurostimulant that is applied through a nasal spray. It is FDA-indicated to treat the signs and symptoms of dry eye.
For more information and to schedule a consultation, please contact our office today to hear more or to schedule a consultation with one of our experienced doctors.